Once a healthcare provider submits a claim to a payer or bills a patient, the A/R process starts. After you receive the payment for your rendered service against a claim, the account is no longer in A/R. Gross accounts receivable is the total amount of money a patient owes to a healthcare provider for the rendered care services. Besides, it is a financial metric that enables providers to oversee revenue streams for a steady cash flow.
How can medical practices manage claim denials effectively?
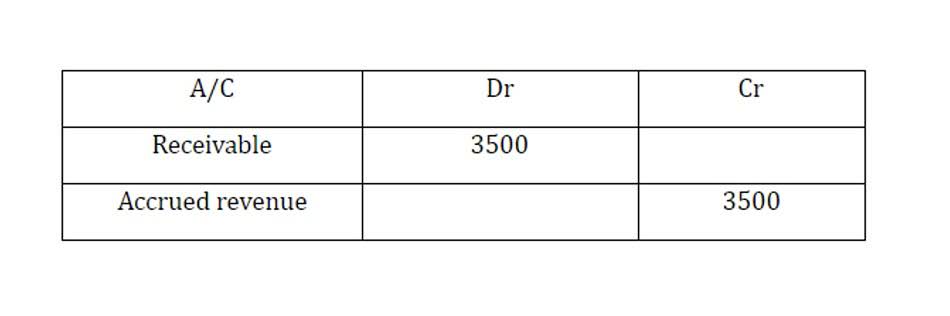
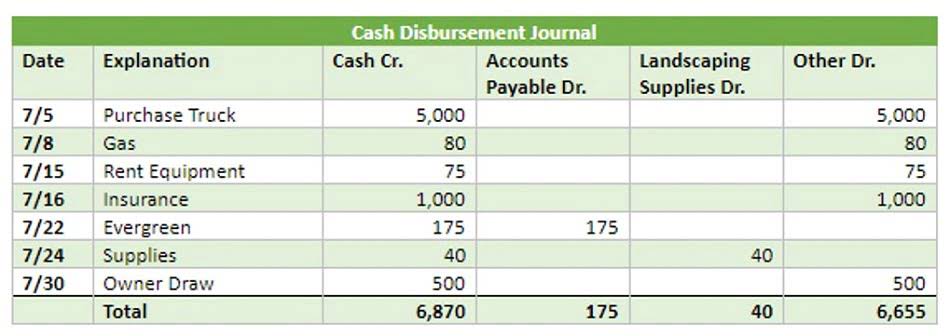
The Data Freshness date/time will let you know how current the information is. Explain the difference between the Cash basis and the Accrual basis of accounting.l 2. Look at the expanded accounting equation and identify which three account types increase with a debit. Look at the expanded accounting equation and identify which three account types increase with a credit. If your practice is largely Medicaid, and the Medicaid agency in your state never pays in less than 90 days, then 86 days considered to be appropriate for Days in AR. Measurement of Account Receivable is called “Days in AR” which represents the average time it takes to collect a bill.
Step # 4 – Follow-up and Track Payments

It defines the unreceived but recognized revenue and is recorded as a current asset in the statement of financial position. It constantly changes as providers perform new care services for patients while reimbursements, write-offs, and adjustments are made to HOA Accounting the billing. AR days are affected by late claim submissions, coding errors, insurance verification issues, and slow follow-ups on outstanding payments. Analytics help identify denial patterns, predict revenue cycles, and improve financial decision-making for healthcare providers. A comprehensive accounts receivable log should provide clear and concise records of patient interactions, including payment dates, amounts due, and any communication with patients regarding their balances.
Health Insurance Providers and Their Role in AR Process
- Analyzing and optimizing A/R reports in health care is critical to making a strong financial structure for your practice.
- Similarly, in the healthcare industry, AR means the patient’s account balance becomes due for payment within a year.
- A great number of medical organizationsutilize expert accounts receivable services to ensure that these payments areappropriately filed, processed, and received.
- Managing accounts receivable in U.S. healthcare requires constant awareness of the constantly changing regulatory compliance landscape.
- The process initiates with the healthcare organization deciding whether they will extend the line of credit to the patient based on their insurance eligibility and benefits verification.
- What they also do is seek the accounts with outstanding charges and then discuss the best strategy for ensuring payment, then finally implementing it until the payment is secured.
Thus, it is recommended that you integrate your electronic health records (EHR) system with a real-time eligibility (RTE) tool to ensure eligibility verification before an encounter. Besides, developing a weekly batch-checking process can also speed up your entire billing workflow. 14% of total denials were due to submitting a claim for excluded services, 8% due to lack of preauthorization, and 2% due to no medical necessity. If outsourcing is necessary, choose a collaborative platform that keeps your team involved in critical billing tasks. No matter what, AR management always requires internal oversight to ensure accuracy and compliance. Staying compliant is a must, but keeping up with constant policy changes feels like a full-time job.
- Accounts Receivable (AR) in medical billing plays a critical role in healthcare revenue cycle management, directly influencing the financial health of healthcare providers and facilities.
- The payment that a patient needs to make but has not yet paid is called patient accounts receivable.
- You can create and configure custom dunning letters from the Patient Accounting Archive.
- A well-organized accounts receivable log facilitates effective communication with patients regarding their outstanding balances.
- At its core, Accounts Receivable (A/R) in healthcare represents the money that healthcare providers are owed for services they’ve delivered.
- The goal is not just about managing accounts receivable for medical practices, but optimizing the process.
It puts the practice in a difficult situation as most patients struggle to understand their financial obligations and how their insurance coverage works. A slower insurance reimbursement process negatively impacts a healthcare facility’s https://babyallbaby.com/assets-liabilities-equity-balance-sheet-basics-2/ cash flow. This issue has a more adverse effect on small practices where resources are limited, specifically financial ones. Outsourcing should be strategic—not just a way to avoid administrative work. Managing claim submissions, reminders, and collections internally is made easier with the use of customized AR software. External billing companies may not fully understand your operations, which causes inefficiencies.
An automated accounts receivable system is scalable and can keep up with your medical practice as it grows without necessarily needing to hire more employees. It allows you to seamlessly accelerate your output for profitable scalability. This is another situation where manual processes and out-of-date systems can cause significant problems. An automated AR system with a centralized dashboard is essential to keep all areas of your accounts receivable processes operating on the same page. Invoices that haven’t yet been paid can’t be classified as income, which can create risky gaps in your operations. Unpaid invoices often lead a business to taking on more debt than accounts receivable log for individual patients is prudent.
- Effective communication strategies, understanding patient financial situations, and offering flexible payment plans can greatly enhance the likelihood of collecting these balances.
- Unpaid invoices often lead a business to taking on more debt than is prudent.
- It is also an important practice in the medical billing process to avoid claim denials.
- Real-time visibility into claim status along with end-to-end claim tracking ensures payments don’t fall through the cracks.
- “Account Receivable” (AR) is a widely used term referring to the amount of money that a customer owes to the company.
Reports on unpaid balances, collection rates, and claim denials highlight problem areas. At its core, Accounts Receivable (A/R) in healthcare represents the money that healthcare providers are owed for services they’ve delivered. This includes everything from hospital stays and surgeries to routine check-ups and specialized treatments.
Let’s delve into what AR entails in medical billing, its significance, and how effective AR management can impact healthcare revenue cycles. Accounts Receivable in medical billing refers to the process of tracking, managing, and collecting payments owed to healthcare providers for medical services provided to patients. When a healthcare provider submits claims to insurance companies or bills patients directly, those unpaid claims or invoices become part of the AR. This amount is expected to be collected within a specific period, often dictated by the provider’s billing terms and agreements with payers.
Thus, your billing office must follow a streamlined process for A/R recovery. Without stringent procedures for payment collection, reducing write-offs is a lost cause. Unnecessary write-offs will be reported as financial losses for the facility, leading to bad debts. The accounts receiver officer (ARO) is responsible for follow-ups and tracking each payment to ensure a steady cash flow. It involves monitoring outstanding balances, initiating follow-up communications, and resolving discrepancies. One of the primary uses of A/R accounts in pharmacies is to offer patients the option of making scheduled payments at a later date.

Provide Interactive Forms
Our streamlined payment posting process enables you to process payment and adjustment transactions on multiple accounts within a batch, allowing for an efficient process when focusing on legacy accounts. This feature is conducive to an environment where billers can focus more of their valuable time on working down their current AR, while not sacrificing revenue from older accounts. Monitoring the percentage of write-offs due to uncollectable balances helps you evaluate your collection process and identify areas where additional resources or strategies may be needed to minimize losses. This metric shows the percentage of collectible revenue you’ve received out of the total allowed charges. A high net collection rate (typically above 95%) reflects strong receivable management practices. This option generally has the most effective accounts receivable collection rates because your system has defined them as the most likely to collect.